Last weekend while we were walking in the countryside we met a young man named Jacob. He told us he went to school in Migori but was called home by his family because his father is quite ill.
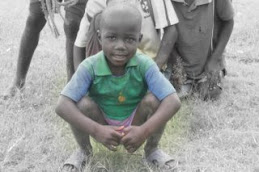
One thing we’ve learned here is that there are no “patient’s rights” per se. The family makes all the decisions for a patient and because women have little or no legal standing or rights, the decisions often fall to the oldest son. That was the case with Jacob. Although he is only 15 he was the one bearing the responsibility for the care of his father.
He told us he planned to walk to Matoso on Monday and try to arrange for his father to be picked up and driven to the closest hospital- St. Camillus- which is an hour away over very rough roads. He told us that his father had been ill for 2 months and was now unable to stand. We suggested that he bring his father to our clinic first to be evaluated first and if he needed to go to the hospital, his transport would be arranged.
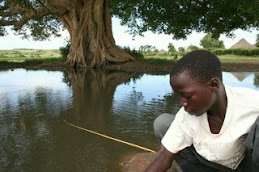
Jacob did bring his father in the morning by lifting him onto a bike and using it as a wheelchair to walk him the 1-2 km to the clinic. As it turned out, the father was a patient in our Patient Support Center (HIV clinic) and was in end stage HIV disease. He was emaciated and extremely weak, his breathing was labored and his heart rate rapid. After evaluating him it was readily apparent that there was nothing the hospital could do for him.
With the family gathered around the patient, Dr. Jeevan explained that their father was dying and he would be given medicine to make him comfortable so he could be taken home to die. Jacob lobbied for his father to be taken to the hospital. He stressed that he was responsible for his father and wanted him to go and that his mother wouldn’t accept him being sent back home without treatment. As we continued to talk it became apparent that he believed that if his father didn’t go to the hospital he would be perceived as a bad son; one that didn’t do enough to save his father. I assured him he was a good son. I explained that it was unlikely that his father would make it to the hospital and he would suffer greatly from the ride over the rough roads.
But what else can I do for my father, he asked? Take him home where he will be surrounded by family and let him die in peace. Take care of your mother. Comfort her. Your father is in God’s hands.
The family acquiesced and after the patient was given a couple doses of pain medicine he was driven home by our staff where he died later that same day.
At a staff meeting that afternoon the subject of end of life care come up. We were all asked if it was better to send a dying person to the hospital, knowing nothing can be done or was it better to send them home to die among family? In America I would know the answer most of my colleagues would give- send them home. So, I was caught off guard when the entire Kenyan clinical staff chose to send the patient to the hospital to die. Their beliefs reflected Jacob’s- that everyone should die in the hospital and sending them home makes the family look as if they didn’t do everything possible for their family member. They would suffer shame in their community.
I immediately became concerned that the care we gave to Jacob and his family wasn’t culturally appropriate. Had we broken our own rule to always listen and respect the wishes of the patient and family? Had I been too coercive?
I talked to the staff about the philosophy of hospice or palliative care but it’s not a concept that has been integrated into patient care in this part of Kenya. Kenyans are more familiar with death than we are in America. They often give a history of losing children, spouses, siblings and parents at early ages due to infectious diseases and other causes but are uncomfortable having them die at home. We ran out of time to continue our discussion but it’s a topic that Paul and I will continue in our educational sessions in the coming months with the hope that we’ll come to understand their culture better while opening their minds to other alternatives to end of life care.




























































































































































































1 comment:
Darcie,
I love your blog!!!!!! This chapter brought a tear to my eye. Have you seen Jacob since? The cultural differences are very interesting as we tend to forget and take things for granted. I would be interested in hearing more about your discussions with the staff regarding some of the issues. You need to publish when you guys get back! Keep on blogging sister!!!
your doctor sis-in-law,
Mary
Post a Comment